Abstract
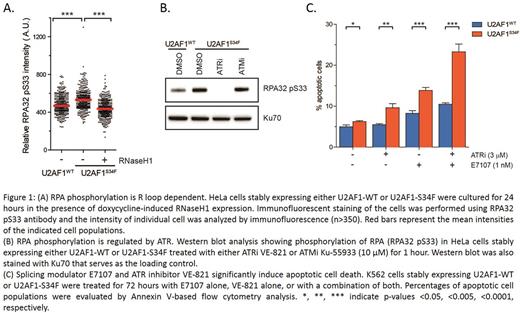
Recurrent missense mutations in genes encoding RNA splicing factors (e.g. U2AF1, SRSF2 and SF3B1) are among the most frequently identified genetic alterations in myeloid malignancies (i.e. myelodysplastic syndromes [MDS], chronic myelomonocytic leukemia, and acute myeloid leukemia). Although genetically-engineered mouse models of the most common mutant alleles (U2AF1-S34F, SRSF2-P95H, SF3B1-K700E) recapitulate the sequence-specific changes in RNA splicing observed inprimary clinical samples carrying these mutations, the precise roles of splicing factor mutations in MDS pathobiology and leukemogenesis are not fully understood. We recently reported that RNA splicing perturbation, either by pharmacologic compounds or by expressing spliceosomal mutations, led to R loop accumulation (Nguyen HD et al, Mol Cell, 2017). R loops are transcription intermediates containing RNA:DNA hybrids and displaced single-stranded DNA (ssDNA). Aberrant R loop accumulation can lead to genomic instability. We showed that Replication Protein A (RPA), a ssDNA-binding protein, localized at R loop and promoted R loop resolution via cooperation with RNaseH1, an enzyme that specifically hydrolyzes RNA:DNA hybrids. Moreover, RPA was phosphorylated at R loops. Given that RPA also interacts directly with the ATR-ATRIP kinase complex, we postulated that the R loop-induced phosphorylation of RPA could be mediated by ATR-ATRIP. Here, we demonstrate that RNA splicing perturbations induce R loop-associated RPA phosphorylation mediated by ATR. HeLa or K562 cells that stably expressed transgenic U2AF1-wild-type (WT) or mutant S34F protein at similar levels to endogenous U2AF1 were selected for this study. To detect phosphorylated-RPA (p-RPA), we performed immunofluorescence staining and western blot analysis, and observed higher levels of p-RPA in U2AF1-S34F expressing cells than in U2AF1-WT expressing cells. Conditional induction of RNaseH1 to remove R loops in S34F mutant cells reduced the elevated p-RPA to a level similar to WT cells (Fig. 1A). In addition, p-RPA was suppressed by an ATR inhibitor (ATRi, VE-821, Fig. 1B), but not an ATM inhibitor (ATMi, Ku-55933), suggesting that p-RPA is triggered by R loops in an ATR-dependent manner. The effect of VE-821 on S34F mutants was validated inan MTS-based cell viability assay. In WT cells, the IC50 of VE-821 was 10.4 +/- 0.8 µM whereas in S34F mutants IC50 dropped significantly to 2.9 +/- 0.2 µM (p < 0.001). These results collectively confirmed that ATR kinase is essential for R loop-associated RPA phosphorylation, and inhibition of ATR activity decreased cell survival. Interestingly, attenuation of R loop formation in S34F mutants by RNaseH1 repressed RPA phosphorylation but did not affect aberrant alternative RNA splicing of five well-validated mutant U2AF1 targets (MED24, KMT2D, BCOR, PICALM, and H2AFY). This finding suggested that mutant U2AF1 triggers two potentially independent pathways: altered RNA processing; and R loop-associated RPA phosphorylation mediated by ATR. Based on these observations, we hypothesized that targeting R loop-associated ATR signaling could be a vulnerability in cells expressing spliceosomal mutations, and that ATR kinase could be a novel therapeutic target in these cells. This notion is distinct from the preferential sensitivity of splicing factor mutant cells to small molecule splicing modulators that has been reported in several recent studies. Furthermore, this notion predicts that further splicing perturbation in mutant cells could enhance the effect of ATRi. To examine this hypothesis, we treated U2AF1-WT and -S34F mutant cells with three conditions: splicing modulator E7107; ATRi VE-821; a combination of both E7107 and VE-821. Upon treatment with E7107 alone, the abundance of R loops and p-RPA were enhanced in the S34F mutants, rendering them more susceptible to ATR inhibition. Consistent with prior observation, RNaseH1 also suppressed the elevated p-RPA levels. Most importantly, by measuring the Annexin V-positive population after 3 days of treatment, the combination of E7107 and VE-821 significantly increased apoptotic cell death in S34F mutants compared to WT (Fig. 1C). Altogether, these findings provide a pre-clinical rationale to test ATR inhibition as a therapeutic strategy in MDS or other myeloid malignancies to target R loop-associated ATR signaling in patients harboring spliceosomal mutations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal